Dr. David Ludwig, MD, recently published a response to my critique of the carbohydrate-insulin-obesity hypothesis. This is good because he defends the idea in more detail than I've encountered in other written works. In fact, his piece is the most scientifically persuasive defense of the idea I can recall.
Before we dig in, I want to emphasize that this is science, not tribal warfare. The goal is to arrive at the best answer, rather than to win an argument. I'm proceeding in good faith, based on my belief that Ludwig and I are both serious people who care about science and human health, and I hope my audience will do the same. That said, let's get to it.
Read more »
Sabtu, 30 Januari 2016
Kamis, 28 Januari 2016
What happens to your immune system when you take statins?
This study was published in the Journal of Leukocyte Biology 2010 Mar;87(3):433-42
Study title and authors:
Opposite effects of simvastatin on the bactericidal and inflammatory response of macrophages to opsonized S. aureus.
Benati D, Ferro M, Savino MT, Ulivieri C, Schiavo E, Nuccitelli A, Pasini FL, Baldari CT.
Department of Evolutionary Biology, University of Siena, Via Aldo Moro 2, 53100 Siena, Italy.
This study can be accessed at: http://www.ncbi.nlm.nih.gov/pubmed/19892847
Phagocytes are white blood cells that protect the body by ingesting harmful toxins, bacteria and dead and dying cells. Cytokines (Tumor necrosis factor alpha (TNFa) and Cyclooxygenase 2 (COX-2), are molecules that trigger and sustain inflammation.
Staphylococcus aureus is a bacterium that is frequently found in the human respiratory tract and on the skin. It is a common cause of skin infections (e.g. boils), respiratory disease (e.g. sinusitis), and food poisoning.
This study investigated the effects of simvastatin on the immune system. The study used human phagocytes that were pretreated with carrier or simvastatin, alone or in association with mevalonate, and subsequently incubated with Staphylococcus aureus.
The study found:
(a) Phagocyte activity was blocked by simvastatin. This effect by simvastatin was reversed by mevalonate.
(b) TNFa and COX-2 activity was enhanced by simvastatin compared with carrier-treated controls. This effect by simvastatin was reversed by mevalonate.
(c) Mevalonate is inhibited by statins.
The results of the study show that statins impair the ability of phagocytes to kill dangerous pathogens, but enhance the production of cytokines that cause excessive inflammation.
Benati concludes: "By enhancing TNFa and COX-2 production while impairing the mechanisms responsible for bacterial killing in macrophages exposed to opsonized bacteria, simvastatin may contribute to establish a state of undesirable, “gratuitous” inflammation in chronically treated patients".
Minggu, 24 Januari 2016
Statins associated with 30% increased risk of death in kidney transplant patients
This paper was published in the Cochrane Database of Systemic Reviews 2009 Apr 15;(2):CD005019
Study title and authors:
HMG CoA reductase inhibitors (statins) for kidney transplant recipients.
Navaneethan SD, Perkovic V, Johnson DW, Nigwekar SU, Craig JC, Strippoli GF.
Department of Nephrology and Hypertension, Glickman Urological and Kidney institute, Cleveland Clinic, Cleveland, OH 44195, USA. navanes@ccf.org
This paper can be accessed at: http://www.ncbi.nlm.nih.gov/pubmed/19370615
This paper assessed the effects of statin therapy on kidney transplant recipients. The paper analysed the results of 14 studies with 3,045 participants that compared death rates of patients.
The analysis found that kidney transplant patients that received statins had a 30% increased risk of death compared to patients who did not take statins.
Senin, 18 Januari 2016
Doctor says statin use could be contributing to rising rates of cataract surgery
This study was published in Ophthalmic Epidemiology 2016 Jan 14:1-6
Study title and authors:
Statin Use and Incident Cataract Surgery: A Case-Control Study.
Study title and authors:
Statin Use and Incident Cataract Surgery: A Case-Control Study.
Erie JC, Pueringer MR, Brue SM, Chamberlain AM, Hodge DO.
Department of Ophthalmology , Mayo Clinic , Rochester , MN , USA.
This study can be accessed at: http://www.ncbi.nlm.nih.gov/pubmed/26766069
Department of Ophthalmology , Mayo Clinic , Rochester , MN , USA.
Jumat, 15 Januari 2016
Analysis of 65 studies reveals low cholesterol levels are significantly associated with increased suicide risk
This study was published in the Journal of Psychiatry and Neuroscience 2016 Jan;41(1):56-69
Study title and authors:
Serum lipid levels and suicidality: a meta-analysis of 65 epidemiological studies.
Study title and authors:
Serum lipid levels and suicidality: a meta-analysis of 65 epidemiological studies.
Wu S, Ding Y, Wu F, Xie G, Hou J, Mao P.
Research Center for Clinical Medicine, the 302nd Hospital of PLA, Beijing, China
This study can be accessed at: http://www.ncbi.nlm.nih.gov/pubmed/26505144
Research Center for Clinical Medicine, the 302nd Hospital of PLA, Beijing, China
Senin, 11 Januari 2016
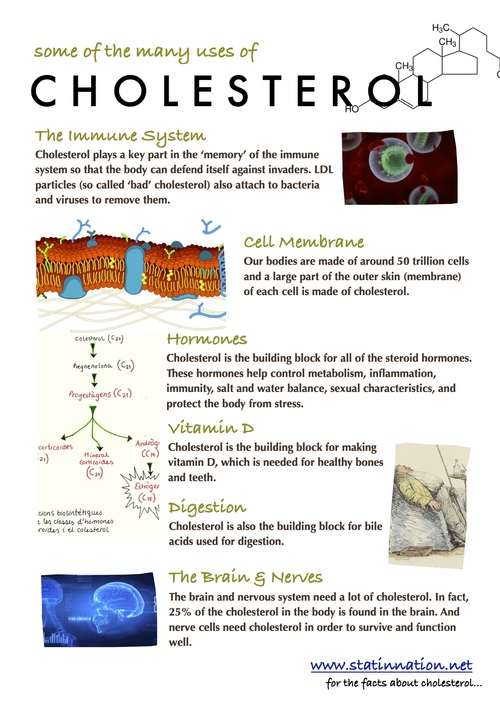
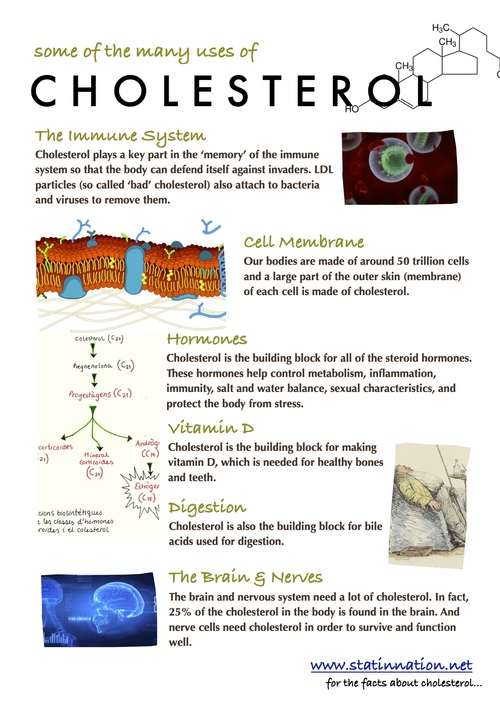
Some of the many uses of cholesterol
This fact sheet regarding cholesterol was created by Justin Smith of Statin Nation.
Justin says: "If we google 'cholesterol' of course we'll find thousands of images portraying it as "artery-clogging", but what about the real functions of cholesterol?
I have created this one page info sheet / poster in an attempt to re-educate about the many things cholesterol is actually used for within the body.
Please send this A4 sized image to anyone you think is afraid of their cholesterol.
Suggestions:
-Print and use as a poster
-Email / hand out to friends and colleagues
-Fix to the front of your statin medication cupboard"
JPEG and PDF versions of the poster can be accessed at: http://www.statinnation.net/blog/2015/12/20/cholesterol-in-the-human-body
Justin says: "If we google 'cholesterol' of course we'll find thousands of images portraying it as "artery-clogging", but what about the real functions of cholesterol?
I have created this one page info sheet / poster in an attempt to re-educate about the many things cholesterol is actually used for within the body.
Please send this A4 sized image to anyone you think is afraid of their cholesterol.
Suggestions:
-Print and use as a poster
-Email / hand out to friends and colleagues
-Fix to the front of your statin medication cupboard"
JPEG and PDF versions of the poster can be accessed at: http://www.statinnation.net/blog/2015/12/20/cholesterol-in-the-human-body
Justin has produced two DVD's that expose the $29billion cholesterol-lowering industry and explains how more than 40 million people have ended up taking a medication that is almost certainly causing them more harm than good.
Sabtu, 09 Januari 2016
Always Hungry? It's Probably Not Your Insulin.
David Ludwig, MD, recently published a new book titled Always Hungry? Conquer cravings, retrain your fat cells, and lose weight permanently. The book is getting widespread media coverage. Ludwig is a professor of pediatrics at the Harvard Medical School and a professor of nutrition at the Harvard School of Public Health. He's a pediatric endocrinologist, but his primary focus is research, particularly the impact of nutrition on hunger, calorie expenditure, and body weight. Although I sometimes disagree with how he interprets evidence, he has made significant and useful contributions to the scientific literature in these areas, and I also support his efforts to find policy solutions to curb the intake of sweetened beverages and other junk foods. In the grand scheme of things, he's an ally in the fight to improve the American diet.
Ludwig has written several high-profile op-ed pieces in recent years, both in the popular press and in scientific journals (1, 2). He argues that our understanding of eating behavior and obesity may be all wrong, and that our focus on calories may be leading us away from the true cause of obesity: hormonal imbalance. And the primary culprit is insulin. You might recognize this idea, because it's similar to the one that science journalist Gary Taubes developed in his book Good Calories, Bad Calories.
According to this view, overeating is irrelevant. We gain fat because our insulin levels are too high, leading our fat tissue to take up too much fat, and other tissues to take up too much glucose, causing our blood energy levels to drop and resulting in fat gain, hunger, and fatigue. The ultimate cause of the problem is the rapidly-digesting carbohydrate and sugar we eat. This idea is encapsulated by Ludwig's quote, "Overeating doesn't make you fat. The process of getting fat makes you overeat" (3).
Here are eleven facts that may make you question this line of reasoning:
Read more »
Ludwig has written several high-profile op-ed pieces in recent years, both in the popular press and in scientific journals (1, 2). He argues that our understanding of eating behavior and obesity may be all wrong, and that our focus on calories may be leading us away from the true cause of obesity: hormonal imbalance. And the primary culprit is insulin. You might recognize this idea, because it's similar to the one that science journalist Gary Taubes developed in his book Good Calories, Bad Calories.
According to this view, overeating is irrelevant. We gain fat because our insulin levels are too high, leading our fat tissue to take up too much fat, and other tissues to take up too much glucose, causing our blood energy levels to drop and resulting in fat gain, hunger, and fatigue. The ultimate cause of the problem is the rapidly-digesting carbohydrate and sugar we eat. This idea is encapsulated by Ludwig's quote, "Overeating doesn't make you fat. The process of getting fat makes you overeat" (3).
Here are eleven facts that may make you question this line of reasoning:
Read more »
Jumat, 08 Januari 2016
Statins associated with a 21% increased risk of non-melanoma skin cancer
This study was published in the British Journal of Cancer 2016 Jan 7
Study title and authors:
Relation of statin use with non-melanoma skin cancer: prospective results from the Women's Health Initiative.
Wang A, Stefanick ML, Kapphahn K, Hedlin H, Desai M, Manson JA, Strickler H, Martin L, Wactawski-Wende J, Simon M, Tang JY.
Department of Dermatology, Stanford University School of Medicine, 450 Broadway Street, Pavilion B, 4th Floor MC 5338, Redwood City, CA 94063, USA.
Selasa, 05 Januari 2016
How Much do You Know About Your Own Brain?
We tend to believe we're aware of what's happening in our own brains, and also in conscious control of our behavior. But a growing body of neuroscience and psychology research demonstrates that most of what happens inside the brain-- including the processes that cause us to select and execute behaviors-- is beyond our conscious awareness. This has important implications for our eating behavior, body weight, and health, as I explore in my upcoming book The Hungry Brain.
Let me give you a straightforward example that illustrates how little of our brain's activity we're aware of. It focuses on information processing by the visual system, which is one of the best-understood systems of the brain. I drew the basic facts of this example from a recent talk by the accomplished neuroscience researcher Marcus Raichle, who studies patterns of activity in the human brain.
Read more »
Let me give you a straightforward example that illustrates how little of our brain's activity we're aware of. It focuses on information processing by the visual system, which is one of the best-understood systems of the brain. I drew the basic facts of this example from a recent talk by the accomplished neuroscience researcher Marcus Raichle, who studies patterns of activity in the human brain.
Read more »
Senin, 04 Januari 2016
Statin use is associated with a 30-36% increased incidence of acute and chronic kidney disease
This study was published in the American Journal of Cardiology December 01, 2015
Study title and authors:
Statin Use and the Risk of Kidney Disease With Long-Term Follow-Up (8.4-Year Study)
Tushar Acharya, MD, Jian Huang, MD, Steven Tringali, DO, Christopher R. Frei, PharmD, MSc, Eric M. Mortensen, MD, MSc, Ishak A. Mansi, MD
This study can be accessed at: http://www.ajconline.org/article/S0002-9149(15)02315-2/abstract
The objective of this study was to determine the association of statin use with incidence of acute and chronic kidney diseases. The study lasted for 8.4 years and included 43,438 individuals, (average age 56 years): 13,626 statin users and 29,812 nonusers. In the study the researchers matched 6,342 statin users with 6,342 nonusers.
The study found:
(a) Statin users had a 30% increased risk of acute kidney injury compared to non-users.
(b) Statin users had a 36% increased risk of chronic kidney disease compared to non-users.
(c) Statin users had a 35% increased risk of nephritis/nephrosis/renal sclerosis compared to non-users.
In a separate analysis, the researchers also matched 3,351 "healthy" statin users with 3,351 nonusers. At the start of the study these individuals were all free of diabetes, chronic kidney disease, cardiovascular disease, and conditions that might limit life expectancy or physical activity.
(d) This separate analysis found that these initially "healthy" statin users had a 53% increased risk of developing chronic kidney disease compared to non-users.
Acharya concluded: "Statin use is associated with increased incidence of acute and chronic kidney disease."
Links to other studies:
Statins increase the risk of diabetes in kidney transplant patients
NSAIDs and statins increase the risk of renal cell carcinoma
The unintended adverse effects of statins in men and women
Study title and authors:
Statin Use and the Risk of Kidney Disease With Long-Term Follow-Up (8.4-Year Study)
Tushar Acharya, MD, Jian Huang, MD, Steven Tringali, DO, Christopher R. Frei, PharmD, MSc, Eric M. Mortensen, MD, MSc, Ishak A. Mansi, MD
This study can be accessed at: http://www.ajconline.org/article/S0002-9149(15)02315-2/abstract
The objective of this study was to determine the association of statin use with incidence of acute and chronic kidney diseases. The study lasted for 8.4 years and included 43,438 individuals, (average age 56 years): 13,626 statin users and 29,812 nonusers. In the study the researchers matched 6,342 statin users with 6,342 nonusers.
The study found:
(a) Statin users had a 30% increased risk of acute kidney injury compared to non-users.
(b) Statin users had a 36% increased risk of chronic kidney disease compared to non-users.
(c) Statin users had a 35% increased risk of nephritis/nephrosis/renal sclerosis compared to non-users.
In a separate analysis, the researchers also matched 3,351 "healthy" statin users with 3,351 nonusers. At the start of the study these individuals were all free of diabetes, chronic kidney disease, cardiovascular disease, and conditions that might limit life expectancy or physical activity.
(d) This separate analysis found that these initially "healthy" statin users had a 53% increased risk of developing chronic kidney disease compared to non-users.
Acharya concluded: "Statin use is associated with increased incidence of acute and chronic kidney disease."
Links to other studies:
Statins increase the risk of diabetes in kidney transplant patients
NSAIDs and statins increase the risk of renal cell carcinoma
The unintended adverse effects of statins in men and women
Langganan:
Komentar (Atom)