 Vilhjalmur Stefansson was an Artic explorer known for his observations on the traditional living Inuit-Eskimo, which he lived together with in the winter of 1906-1907 in the Mackenzie Delta of Canada. Stefansson asserted that during this time he subsisted on traditional Inuit fare, based almost exclusively on flesh. In part based on less than extensive observations of the health of the Inuit, Stefansson hypothesized that a number of chronic and degenerative diseases, including cancer are diseases of civilization which can be prevented by adherence to a pre-modern diet and lifestyle. However, Stefansson did not suggest that only flesh based dietary patterns, such as that consumed by the traditional living Inuit, but also primarily vegetarian diets, such as that consumed by the Hunza may protect against such diseases.1
Vilhjalmur Stefansson was an Artic explorer known for his observations on the traditional living Inuit-Eskimo, which he lived together with in the winter of 1906-1907 in the Mackenzie Delta of Canada. Stefansson asserted that during this time he subsisted on traditional Inuit fare, based almost exclusively on flesh. In part based on less than extensive observations of the health of the Inuit, Stefansson hypothesized that a number of chronic and degenerative diseases, including cancer are diseases of civilization which can be prevented by adherence to a pre-modern diet and lifestyle. However, Stefansson did not suggest that only flesh based dietary patterns, such as that consumed by the traditional living Inuit, but also primarily vegetarian diets, such as that consumed by the Hunza may protect against such diseases.1 The term diseases of civilization, which Stefansson has contributed to the popularization of is frequently referred to by proponents of Low-Carb, Paleo, Primal and Weston A. Price Foundation type diets. Many of these proponents have extrapolated limited suggestive evidence that obesity, type 2 diabetes, coronary heart disease, certain cancers, and a number of other chronic and degenerative diseases were uncommon during the Paleolithic period to suggesting that foods derived from naturally raised, grass-fed animals, as was consumed by Paleolithic humans must therefore somehow provide protection against these so-called diseases of civilization. Many of these proponents have also claimed that a vast number of scientific studies that have been used as evidence to conclude that animal foods increase the risk of such diseases have been complicated by confounding of other unhealthy foods and lifestyle factors, or by the use of unnaturally raised animal foods. This series of posts will examine the evidence to help determine whether these claimed confounding variables can actually explain the evidence linking animal foods with certain chronic and degenerative diseases, often referred to as diseases of civilization, but also as western diseases, lifestyle diseases and diseases of affluence.
In 1928, Stefansson and his colleague Karsten Anderson participated in a monitored experiment partly funded by the meat industry in which they consumed a flesh exclusive diet for the period of one year. Although the researchers concluded that these two men were in good health throughout the experiment, Anderson experienced a severe elevation in blood cholesterol, with measurements as high as 800 mg/dl on one occasion, which returned to pre-experiment levels after resuming a higher carbohydrate diet.2 A glucose tolerance test carried out immediately after the termination of the meat based experiment showed a marked rise in blood sugar in both men compared to a subsequent test carried out after resuming a higher carbohydrate diet. Glucose was detected in the urine of Anderson in the test following the meat based experiment, a marker of untreated diabetes. This abnormality was not detected in the subsequent test after resuming a higher carbohydrate diet.3
Short-term experiments such as this cannot provide adequate insight into the long-term consequences of following such a diet, as it can take many decades for diseases caused by exposure to harmful substances to become clinically significant. For example, the greatest risk of excess death from radiation-related solid cancers among the atomic bomb survivors of Hiroshima and Nagasaki was more than half a century after exposure.4 Furthermore, other flesh based experiments have resulted in considerably more unfavorable outcomes. For example, in 1906, Russell noted an even earlier experiment:
A recent instance occurred in South Africa, where about twenty natives out of some hundreds who were supplied with a large amount of flesh, as an experiment, by mine-owners, died, and many others were ill.5
Cardiovascular Disease in Ancient Civilizations
 |
| The traditional living Inuit's were certainly not immune from atherosclerosis |
Contrary to claims of the traditional living Inuit being immune from cardiovascular disease, evidence of severe atherosclerosis has been identified in several frozen mummies of Alaskan Inuit dating back to 400 CE and 1520 CE, both instances predating European contact.7 8 Atherosclerosis has also previously been identified in several artificially prepared mummies of Aleut-Unangan hunter gatherers who lived in the 18th century in the Aleutian Islands in Alaska.9 10 Recently the HORUS study, which examined an additional five recovered mummies of Unangan hunter gatherers who lived in the mid and late 19th century found definite evidence of atherosclerosis in several major arteries in all three who were over the age of 25.11
When considering the findings from all of these Alaskan Inuit and Aleut mummies it becomes evident that these Alaskan natives likely experienced a greater incidence of atherosclerosis, especially given the young mean age compared to the three other ancient populations studied in the HORUS study. Unlike the Alaskan natives, these other three populations, which were the ancient Egyptians, ancient Peruvians and Ancestral Puebloans practiced agriculture and consumed grains.
In addition to evidence of atherosclerosis from native Alaskan mummies, reports from medical officers provide further evidence of unfavorable rates of cardiovascular disease among the Inuit before the rapid transition to the western diet. In 1940, based on decades of clinical practice and reviewing reports of medical officers dating all the way back 175 years ago, Bertelsen, who is considered the father of Greenland epidemiology stated in regards to the mortality patterns among the Greenland Inuit that:
...arteriosclerosis and degeneration of the myocardium are quite common conditions among the Inuit, in particular considering the low mean age of the population.12
Bjerregaard and colleagues performed a literature review for studies addressing the incidence of atherosclerosis and cardiovascular disease among the Inuit of Alaska, Canada and Greenland spanning from the 1930s to more recent decades. The researchers found that the incidence of atherosclerosis was generally similar to that of other western populations that suffered from high rates of cardiovascular disease. Mortality from stroke was found to be even higher, and mortality from all cardiovascular diseases combined was found to be similar or even higher among the Inuit. The researchers also found that mortality from coronary heart disease among the Inuit was not significantly different after adjusting for ill-defined causes of cardiovascular death, suggesting that the substantial proportion of cardiovascular deaths being classified as ‘garbage codes’, particularly in Greenland may have hidden a significant portion of deaths from coronary heart disease. The researchers concluded:
The mortality from all cardiovascular diseases combined is not lower among the Inuit than in white comparison populations. If the mortality from IHD [ischemic heart disease] is low, it seems not to be associated with a low prevalence of general atherosclerosis. A decreasing trend in mortality from IHD in Inuit populations undergoing rapid westernization supports the need for a critical rethinking of cardiovascular epidemiology among the Inuit and the role of a marine diet in this population.12
A similar phenomenon to the misclassification of deaths from coronary heart disease among the Inuit populations has also been observed in France, which may largely explain the so-called French Paradox. Data from the World Health Organization MONICA Project suggests that the official mortality statistics for France significantly underreport deaths from cardiovascular disease compared to other countries, with deaths from coronary heart disease being underestimated by 75%. Other reports suggest that this is likely explained by a much higher rate of French doctors classifying deaths as due to ‘other causes’ than in other countries.13 14
It has been observed that among the Alaskan Inuit a higher intake of saturated fat is associated with elevated blood pressure, insulin resistance, glucose intolerance and carotid atherosclerosis, suggesting that the traditional Inuit foods relatively rich in saturated fat were likely to have been detrimental to the cardiovascular health of the Inuit.15 16 17 It has also been observed that among Alaskan Inuit elevated LDL cholesterol is associated with a greater than fourfold increased risk of cardiovascular disease.18 Furthermore, rheumatic disorders that have been linked to cardiovascular disease, such as gout and rheumatoid arthritis have been found to be just as, or even more common among the Eskimo populations compared to that of the general North American population.19 20 Established risk factors, a number of which are likely adversely affected by the traditional Inuit diet can probably in part explain the evidence of severe atherosclerosis and unfavorable rates of cardiovascular disease observed among the traditional living Inuit and Aleut populations.
It has been observed that among the Alaskan Inuit a higher intake of saturated fat is associated with elevated blood pressure, insulin resistance, glucose intolerance and carotid atherosclerosis, suggesting that the traditional Inuit foods relatively rich in saturated fat were likely to have been detrimental to the cardiovascular health of the Inuit.15 16 17 It has also been observed that among Alaskan Inuit elevated LDL cholesterol is associated with a greater than fourfold increased risk of cardiovascular disease.18 Furthermore, rheumatic disorders that have been linked to cardiovascular disease, such as gout and rheumatoid arthritis have been found to be just as, or even more common among the Eskimo populations compared to that of the general North American population.19 20 Established risk factors, a number of which are likely adversely affected by the traditional Inuit diet can probably in part explain the evidence of severe atherosclerosis and unfavorable rates of cardiovascular disease observed among the traditional living Inuit and Aleut populations.
In the HORUS study it was found that two of the four Ancestral Puebloan who lived in southwestern United States dating between 1500 BCE and 500 CE exhibited probable evidence of atherosclerosis, the two other both being under the age of 30. These Ancestral Puebloans were identified as being from a time when they were transitioning from hunter-gatherers to farmer-foragers, and were likely to have relied on hunted animal foods to supply at least a modest portion of their diet. An additional Ancestral Puebloan mummy aged 18-22 found from a later period after a greater transition towards agriculture did not exhibit any evidence of atherosclerosis.11
In the HORUS study the ancient Egyptian mummies exhibited the next greatest frequency of atherosclerosis, with 29 (38%) of the 76 of the mummies exhibiting at least probable evidence of atherosclerosis.11 In their book Protein Power, Michael and Mary Eades assert that the ‘diet of the average [ancient] Egyptian consisted primarily of carbohydrates’, which they suggest was ‘a veritable nutritionist’s nirvana… rich in all the foods believed to promote health and almost devoid of saturated fat and cholesterol'. These authors go on to suggesting that the carbohydrate rich diet of the ‘average Egyptian’ which they describe as being based on whole-grain wheat and barley supplemented by a variety of fruits, vegetables, legumes, nuts and some goats milk is responsible for the atherosclerosis and obesity exhibited by the ancient Egyptian mummies.21
There is much evidence that casts doubt on these authors description of the diets of the ancient Egyptian mummies. For example, Macko and colleagues have shown that isotope analyses of the amino-acid composition of hair from the ancient Egyptian mummies far more closely resemble that of modern westerners following an omnivorous diet than a vegetarian, and especially vegan diet.22 In addition, David and colleagues showed that evidence from hieroglyphic inscriptions on ancient Egyptian temples suggest that the elites of ancient Egyptian society, being those who were primarily mummified consumed a diet rich in flesh and saturated animal fat. These researchers addressed the confusion surrounding the diet and atherosclerosis of the ancient Egyptian mummies, asserting:
 |
| The authors of Protein Power suggest that complex carbohydrates, such as wheat made the ancient Egyptians obese |
There is much evidence that casts doubt on these authors description of the diets of the ancient Egyptian mummies. For example, Macko and colleagues have shown that isotope analyses of the amino-acid composition of hair from the ancient Egyptian mummies far more closely resemble that of modern westerners following an omnivorous diet than a vegetarian, and especially vegan diet.22 In addition, David and colleagues showed that evidence from hieroglyphic inscriptions on ancient Egyptian temples suggest that the elites of ancient Egyptian society, being those who were primarily mummified consumed a diet rich in flesh and saturated animal fat. These researchers addressed the confusion surrounding the diet and atherosclerosis of the ancient Egyptian mummies, asserting:
It is important to point out that there was a marked difference between the mainly vegetarian diet most Egyptians ate and that of royalty and priests and their family members whose daily intake would have included these high levels of saturated fat. Mummification was practised by the elite groups in society, ensuring that their remains have survived to provide clear indications of atherosclerosis; by contrast, there is a lack of evidence that the condition existed among the less well-preserved remains of the [mainly vegetarian] lower classes.23
The findings of a lower incidence of atherosclerosis among the lower classes of ancient Egypt who subsisted primarily on a carbohydrate-rich vegetarian diet are consistent with observations in Egypt in the early 20th century. In 1934, Rosenthal asserted:
Of interest is the report of Ismail in Egypt, who has communicated that among his private patients, whose diet is similar to that of the Europeans, the incidence of atherosclerosis is high, while in his hospital practice, composed mainly of natives, who subsist largely on a carbohydrate diet, the incidence of atherosclerosis is low.24
It is clear that the authors of Protein Power have confused the diet of the elites of the ancient Egyptian society, who certainly cannot be considered as the 'average Egyptian' with the largely vegetarian diet of the of the lower classes who exhibit a lack of atherosclerosis, and which scant evidence suggests were obese. The findings from ancient Egyptian mummies do not support the claimed benefits of a low carbohydrate, high saturated fat diet promoted by these authors.
In the HORUS study, despite having the highest mean age, nearly 10 years older than that of the Unangan and Ancestral Puebloans mummies, the ancient Peruvians exhibited the lowest incidence of atherosclerosis, being evident in 13 (25%) of 51 of the mummies. Compared to these other studied ancient populations, the Peruvians likely relied more on staple plant foods, such as corn, beans and tubers, although did consume some domesticated and hunted animals.11
The researchers of the HORUS study suggested that exposure to smoke from fire used for cooking and25
heating may help explain some of the degree of atherosclerosis identified in these ancient populations. However, the description of the use of fire for cooking in ancient Egypt provided by these researchers would apply primarily to the lower classes of ancient Egypt which exhibit a lack of atherosclerosis, rather than the mummified elites that these researchers examined who would typically have had servants to cook for them.
heating may help explain some of the degree of atherosclerosis identified in these ancient populations. However, the description of the use of fire for cooking in ancient Egypt provided by these researchers would apply primarily to the lower classes of ancient Egypt which exhibit a lack of atherosclerosis, rather than the mummified elites that these researchers examined who would typically have had servants to cook for them.
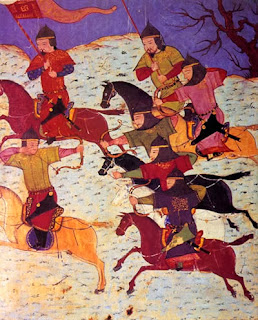 |
Gout was known to be common among the Mongols of the Golden Horde |
Another population that have historically been documented to subsist almost exclusively on a diet derived from grass-fed, free-ranging animals are the largely nomadic Mongolians. John of Plano Carpini who visited the Mongols in the mid-13th century noted:
Smith reviewed the literature regarding the health of the Mongols from the 13th century and noted that a number of unfavorable cardiovascular risk factors, including obesity and gout were both common disorders. Smith went on to state:[The Mongols] have neither bread nor herbs nor vegetables nor anything else, nothing but meat… They drink mare’s milk in very great quantities if they have it; they also drink the milk of ewes, cows, goats and even camels.28
Cardio-vascular problems, although not then subject to diagnosis, may be suspected as well.29In 1925, Kuczynski reported on the nomadic pastoralists of the Kirghiz and Dzungarian Steppes in Central Asia and northern China that were of Mongolian descent. Similar to the observations of the diet of the nomadic Mongols of the 13th century, Kuczynski observed that these nomadic pastoralists subsisted almost exclusively on enormous quantities of meat and milk from grass-fed, free-ranging animals. Other authors have also come to the same conclusions regarding the composition of the diet of the nomadic pastoralists of the Central Asian Steppes. For example, Tayzhanov asserted:
Similarly, Barfield asserted:…the people [of the steppe] lived exclusively on meat, fat and sour milk. Bread was added only later and even then some households did not adopt or consume this food.30
These findings suggest that the diet of these nomadic pastoralists of the Central Asian Steppes was almost exclusively animal based, virtually devoid of grains, legumes and refined carbohydrates. This should make these populations also suitable to study the hypothesis that naturally raised animal foods protect against cardiovascular disease. However, not only did Kuczynski observe that these nomadic pastoralists suffered from high rates of obesity and gout similar to the Mongols of the 13th century, Kuczynski's observations further extended to the diagnosis of cardiovascular disease and other dietary related disorders. Kuczynski asserted:In good legendary style, the pure Central Asian nomads eat only meat, marrow, and milk products {preferably ferments}. They despise farmers, farming, and grain…31
It was also observed that in the 1960s the prevalence of coronary heart disease among the nomadic pastoralists in Xinjiang in northern China who consumed large quantities of animal fat from grass-fed, free-ranging animals was more than seven times higher than that of other populations both within Xinjiang and throughout China which consumed significantly less animal fat.33 These observations support the suggestion that cardiovascular disease was common among the Mongols of the 13th century who subsisted almost exclusively on a diet based on grass-fed, free-ranging animals.They get arteriosclerosis in an intense degree and often at an early age as shown by cardiac symptoms, nervous disordes, typical changes of the peripheral vessels, nephrosclerosis and, finally, apoplectic attacks. Even in men thirty-two years old I frequently observed arcus senilis.32
Dispelling Grass-Fed Fairy Tales
These findings from populations living before the 20th century suggest that similar to the findings from people studied in more modern times, a greater intake of minimally refined plant foods strongly predicts a lower prevalence of atherosclerosis and cardiovascular disease. These findings cast doubt on the hypothesis that foods from organic, naturally raised animals protect against cardiovascular disease compared to staple plant foods. Furthermore, these findings suggest that the traditional living populations that relied predominantly on naturally raised animal based foods suffered from complications related to cardiovascular disease at a relatively young age and are poor role models for health.
Future posts in this series will further address how naturally raised animal foods influence cardiovascular disease, as well as other so-called diseases of civilization.
Please post any comments in the Discussion Thread.











